Hysterectomy Risks and Benefits: A Complete Guide by Leading Obstetricians & Gynecologists
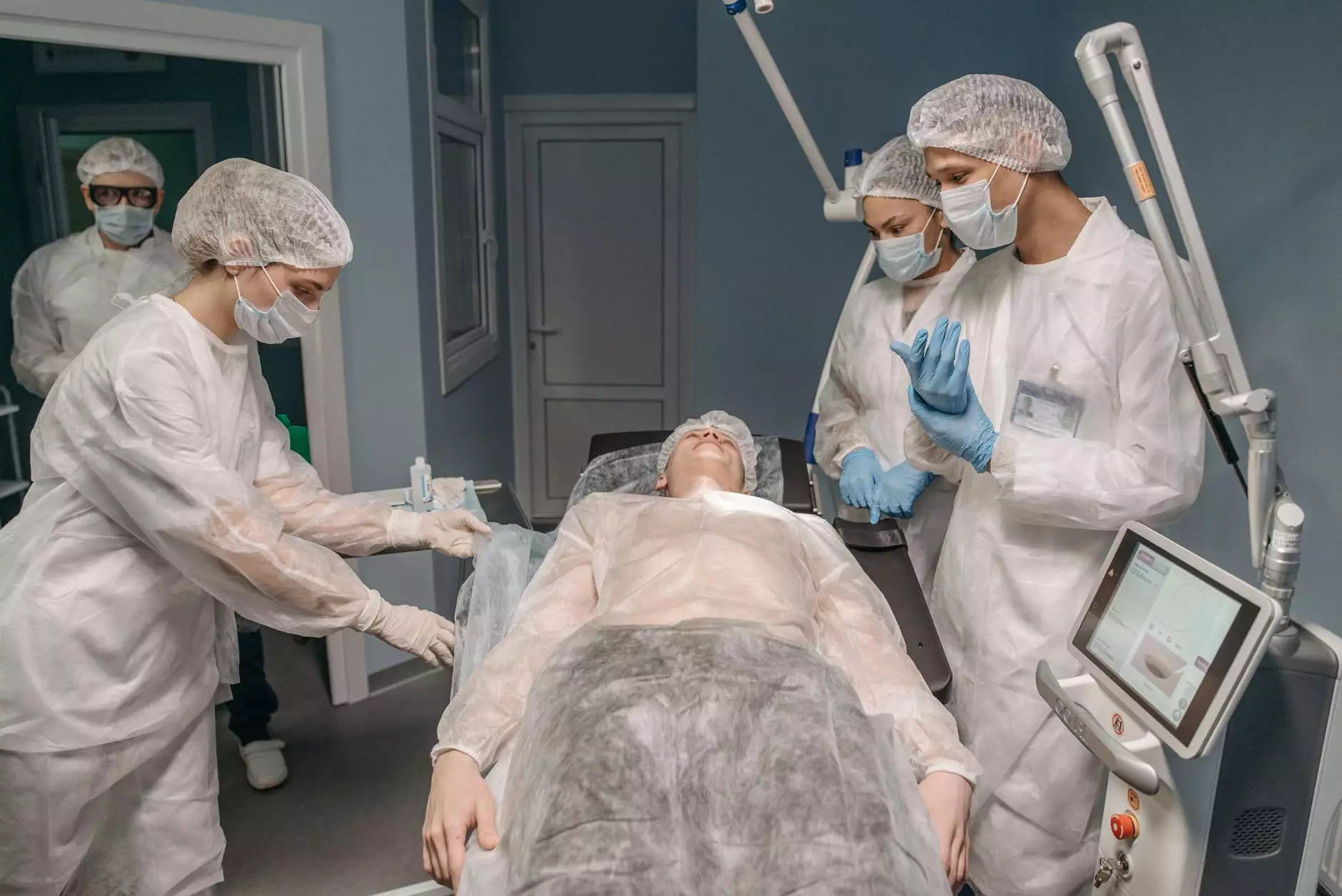
Understanding the intricacies of hysterectomy is essential for women who are considering this transformative surgical procedure. As one of the most common gynecological surgeries, a hysterectomy can significantly impact a woman's health and quality of life. This comprehensive guide, authored by experienced obstetricians and gynecologists from drseckin.com, aims to provide detailed information about the risks and benefits of hysterectomy, helping women make informed decisions about their healthcare.
What Is a Hysterectomy?
A hysterectomy is a surgical procedure that involves the removal of the uterus, with or without the removal of surrounding structures such as the cervix, ovaries, and fallopian tubes. This procedure is performed for various medical indications, including fibroids, abnormal bleeding, endometriosis, uterine prolapse, and certain cancers.
There are several types of hysterectomy, including:
- Subtotal (partial) hysterectomy: Removal of the upper part of the uterus while preserving the cervix.
- Total hysterectomy: Removal of the entire uterus, including the cervix.
- Radical hysterectomy: Removal of the uterus, tissue around the cervix, and part of the vagina, typically performed for cancer treatment.
- Minimally invasive hysterectomy: Includes laparoscopic and robotic-assisted procedures, often offering quicker recovery times.
Common Reasons for Considering a Hysterectomy
Women may consider a hysterectomy for several medical conditions, such as:
- Uterine fibroids causing pain, bleeding, or pressure symptoms
- Abnormal uterine bleeding unresponsive to other treatments
- Endometriosis resulting in severe pain and infertility issues
- Pelvic organ prolapse leading to discomfort or urinary issues
- Cancer of the uterus, cervix, or ovaries
- Adenomyosis causing heavy bleeding and pain
The Benefits of Hysterectomy
While a hysterectomy may seem invasive, it offers numerous benefits when performed appropriately and for suitable indications:
- Symptom Relief: Significant reduction or resolution of symptoms like heavy bleeding, pelvic pain, and pressure sensations.
- Definitive Treatment: Eliminates the source of certain cancers and other severe gynecological conditions.
- Improved Quality of Life: Restores comfort, sleep, and daily functioning for affected women.
- Prevention: In cases of pre-cancerous conditions or high risk of gynecologic cancers, hysterectomy can be a preventative measure.
- Enhanced Psychological Wellbeing: When symptoms are severe, relief can significantly improve mental health and emotional resilience.
Understanding the Risks Associated with Hysterectomy
Despite its benefits, a hysterectomy carries potential risks that must be carefully considered. These risks can vary depending on the patient’s age, overall health, and the extent of the surgery.
Common Surgical Risks
- Bleeding: Excessive blood loss requiring transfusion or additional interventions.
- Infection: Postoperative infections can occur at incision sites or internally, requiring antibiotics or further procedures.
- Reactions to Anesthesia: Adverse responses can present during or after surgery.
- Damage to Adjacent Organs: Unintentional injury to the bladder, ureters, or bowel during surgery.
Long-term Risks and Considerations
- Hormonal Changes: Removal of ovaries (oophorectomy) induces menopause, leading to hot flashes, osteoporosis, and cardiovascular risks.
- Psychological Impact: Some women experience feelings of loss or changes in sexuality post-surgery.
- Potential for Pelvic Floor Issues: Altered pelvic support may lead to prolapse or urinary incontinence in some cases.
- Emerging Risks: Studies suggest a slight increase in cardiovascular disease and cognitive changes in women who undergo early hysterectomy.
Choosing the Right Type of Hysterectomy: Personalized Medical Decision-Making
Deciding on a hysterectomy involves a nuanced understanding of individual health status, the specific medical condition, and personal preferences. Leading obstetricians and gynecologists emphasize a personalized approach, often exploring less invasive alternatives before recommending surgery.
Factors influencing the decision include:
- Severity and type of gynecological issues
- Patient’s age and overall health
- Potential impact on hormonal balance
- Future fertility desires
- Risks associated with anesthesia and surgery
Advanced diagnostic tools, such as ultrasound, MRI, and minimally invasive procedures, assist physicians in tailoring the treatment plan best suited for each patient.
Innovative and Minimally Invasive Approaches to Hysterectomy
Modern medicine offers less invasive options, reducing recovery times and minimizing complications. These include:
- Laparoscopic hysterectomy: Small incisions and camera-guided removal of the uterus.
- Robotic-assisted hysterectomy: Enhanced precision and visualization with robotic technology.
- Vaginal hysterectomy: Removing the uterus through the vaginal canal, often used for prolapse or benign conditions.
These approaches are associated with shorter hospital stays, reduced pain, and quicker return to normal activities.
Preoperative Preparation and Postoperative Care
Successful outcomes depend on thorough preoperative assessment and diligent postoperative management. Key steps include:
- Comprehensive medical evaluation, including blood tests and imaging
- Discussing anesthesia options and addressing patient concerns
- Planning for recovery, including activity restrictions and wound care
- Monitoring for complications such as infection or bleeding
- Long-term follow-up, especially if ovaries are removed, to manage menopausal symptoms and bone health
Informed Decisions: The Role of Expert Medical Advice
Consulting with experienced gynecologists at a reputable facility like drseckin.com is crucial. They provide personalized advice, detailed explanations of the risks and benefits, and ensure that women understand all surgical options.
Empowered decision-making involves understanding the implications, exploring alternative treatments, and evaluating the timing and necessity of a hysterectomy.
Final Thoughts on Hysterectomy Risks and Benefits
Hysterectomy remains a vital surgical intervention for numerous gynecological conditions, offering relief and preventive benefits for many women. However, like any major surgery, it is associated with specific risks that require careful consideration and expert management.
Advances in surgical techniques and personalized care models continue to improve outcomes, making hysterectomy a safer and more effective option than ever before.
Women contemplating this surgery should seek consultation from leading obstetricians and gynecologists to weigh the risks and benefits based on their unique circumstances. Ultimately, informed choices lead to better health and a more positive outlook for the future.
For comprehensive guidance and personalized consultation, visit drseckin.com.









